http://www.physorg.com/news/2010-11-black-children-die-neuroblastoma.html

The study also found that black and Native American children are more likely to have the high-risk form of the disease and show signs of resistance to modern treatment. Those biological characteristics suggest that genetic factors contribute to the outcome disparities found for neuroblastoma.
"Disparities in outcome according to race do exist in neuroblastoma," said Susan Cohn, MD, professor of pediatrics at Comer Children's Hospital at the University of Chicago Medical Center and senior author of the study. "There are racial cohorts of patients who do more poorly than the white population."
The analysis, published online November 22 by the Journal of Clinical Oncology, uses data collected by the Children's Oncology Group (COG), a partnership of more than 200 clinical sites in North America. Because neuroblastoma is a rare cancer, with only 650 new cases each year in the United States, the large coalition was essential to follow enough patients to answer questions about race and ethnicity, Cohn said.
"This kind of study has largely been impeded by the very small numbers of patients that we see, and the small numbers of minorities within that subset," Cohn said. "Through the COG infrastructure, we are able to collect data on the vast majority of patients who are diagnosed with neuroblastoma in North America. It's a much richer data set."
A subject pool of 3,500 children diagnosed between 2001 and 2009 enabled a research group led by Cohn and Tara Henderson, MD, MPH, Assistant Professor of Pediatrics, to compare children of different races on neuroblastoma risk and survival. While 75 percent of white and Hispanic patients survived five years after diagnosis, only 67 percent of black patients, 63 percent of Asian patients, and 39 percent of Native American patients survived to that point.
Patients diagnosed with neuroblastoma are classified as having low-risk, intermediate-risk, or high-risk disease based on a number of clinical and biological factors. Black children in the study had a higher prevalence of high-risk disease (57 percent) compared to white children (44 percent). Black patients also more frequently displayed individual predictors of high-risk disease, such as older age at diagnosis, stage 4 disease, and unfavorable histology.___________________________________
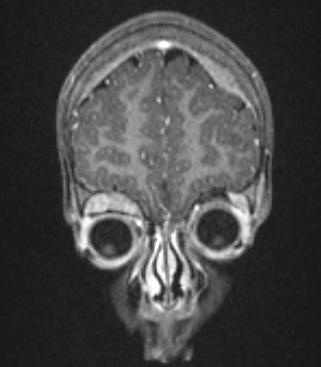
An MRI of a 2-year-old girl with known neuroblastoma
___________________________________
"By definition, if you are older and have advanced stage disease, you are at high risk for relapse and more difficult to cure," Cohn said. "The major reason why the black patients do worse is because there are more of them in this high-risk group."
Another disparity emerged when researchers looked at the timing of post-treatment events such as cancer relapse or progression. After two event-free years following diagnosis, black patients with high-risk disease were significantly more likely to suffer a "late-occurring" event than white patients. This observation suggests black patients are more likely to have residual cancer after therapy, Cohn said.
Follow-up studies are underway to look for genetic factors that may predispose black children to high-risk forms of neuroblastoma and chemotherapy resistance. To do so, Cohn's group will partner with the University of Chicago pharmacogenetics team of M. Eileen Dolan, PhD, professor of medicine and Nancy Cox, PhD, professor of medicine.
The team will look for gene variations associated with chemotherapy resistance and the development of clinically aggressive high-risk disease in black and white neuroblastoma patients. The team will work with genome-wide association data (GWAS) provided by John Maris, MD, professor of medicine at the Children's Hospital of Pennsylvania, which identified predictors of high-risk neuroblastoma in a subject pool of white children.
"Our long term goal is to utilize this kind of information to develop individualized therapy," Cohn said. "For example, if you know that a particular patient has a genotype that is associated with resistance to a specific chemotherapeutic agent, you might either modify the dose or treat the patient with a different agent."
The study also offers a potentially unique example of a disparity due primarily to biological, rather than socioeconomic factors. In many adult cancer types, the survival gap between white and minority patients is often attributed to factors such as diminished access to health care, delayed diagnosis, and poorer quality treatment.
But in neuroblastoma, this is less likely to be an issue. Low-risk cancers rarely progress to a higher risk with time, Cohn said, making a delayed diagnosis less likely to affect outcome. Furthermore, treatment for high-risk neuroblastoma – including intravenous chemotherapy, stem cell transplant, and radiation – is largely administered in a hospital setting, removing the effect of compliance, such as missing oral doses of medications at home.
"In many cancers, disparities in outcome appear to be largely due to differences in socio-economic status and environment. For example, the lack of ability to be seen by a doctor in a timely manner and get appropriate care significantly impacts survival," Cohn said. "While multiple factors are also likely to contribute to the disparities we observed in children with neuroblastoma, genetic factors are likely to contribute to the increased prevalence of high-risk tumors in the black cohort, which is quite unique."
Provided by University of Chicago Medical Center
CLICK HERE TO GO BACK TO MAIN PAGE................or HERE TO GO HOME

No comments:
Post a Comment